Author: Lisa Cheek, PT, DPT, CLT-LANA
Everything you wanted to know about the pelvic floor but were afraid to ask.
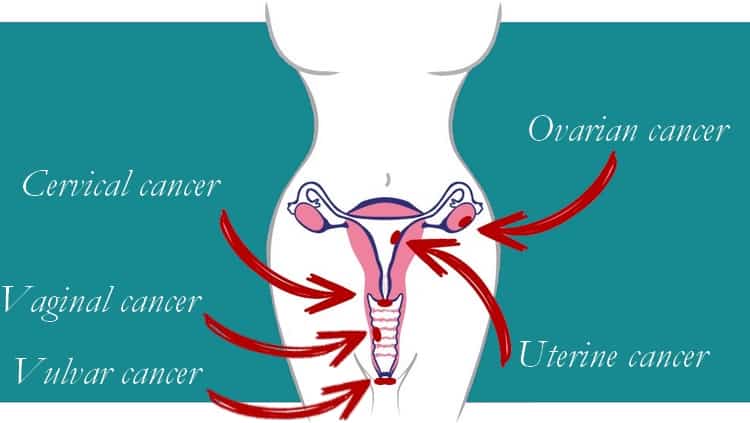
The pelvic floor is an important group of muscles that lives in the bottom of the pelvic bowl. These muscles influence bladder, bowel, and sexual function, and play an important role in spinal stability. They even help us breath! The pelvic floor is constantly working, and yet many people have no idea that this group of muscles even exists. Patients often come to us with preconceived notions of pelvic floor health. You may have heard that we should all be doing our Kegels daily, or that leaking a little urine when you sneeze is “normal”. It can be difficult to separate pelvic floor fact from fiction, especially in the information age. It is well documented that gynecologic cancers (endometrial, ovarian, cervical, vulvar, etc.) and their subsequent treatments can have a big impact on pelvic floor function, which can in turn negatively impact quality of life. We hope to help you learn about the pelvic floor and its typical function, how this can be affected by cancer treatments, and how you can take control and manage pelvic floor dysfunction.
What is the pelvic floor, and what does it do?
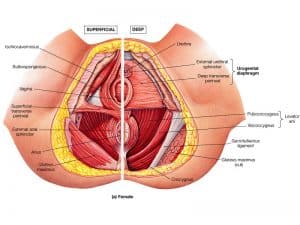
As previously mentioned, the pelvic floor lives at the bottom of the pelvis and is made of several layers of muscles that extend from your pubic bone to your tailbone. It is made of three layers of muscle which extend from your pubic bone back to your tailbone, and out to your hips on the side. The pelvic floor has a few main functions:
1. Sphincteric– The pelvic floor muscles form sphincters around the urethra, vagina, and rectum. They act as the gatekeepers from the pelvic bowl to the outside world. They play an important role in maintaining urinary and fecal continence, and supporting sexual function.
2. Support– Think of the pelvic floor as a hammock for the pelvic organs: the bladder, uterus, and descending colon. They provide support for these organs as we move around in our daily lives.
3. Sexual function– The muscles of the pelvic floor play an important role in sexual arousal and orgasm. They help maintain bloodflow to vaginal region, and contract rhythmically to enhance sexual pleasure.
4. Stabilization– There are four muscles that form a canister of stability in your midsection and keep your spine and pelvis stable, including: the pelvic floor, the diaphragm, the transverse abdominis (the “weight belt” muscle), and the multifidi on the spine. These muscles all need to work together to provide stability and support normal function.
When the muscles of the pelvic floor are working together and at the right time, they perform all the functions listed above. However, this is not always the case. Pelvic floor dysfunction can happen to anyone, regardless of gender, age, or health status. Symptoms of pelvic floor dysfunction can include urinary incontinence, pelvic organ prolapse, pelvic pain, bowel dysfunction, and beyond.
How does treatment for cancer affect the pelvic floor?
Treatment for gynecologic cancers depends on the tumor size, location, and stage. Surgical treatments may involve local excision, tumor debulking, hysterectomy (removal of the uterus), salpingo-oophrectomy, and removal of pelvic lymph nodes. These procedures can directly affect the pelvic floor through scar tissue restriction and swelling, and may also have an indirect effect due to hormonal changes associated with removal of ovaries.1 Adjuvant therapies, such as chemotherapy and radiation, may also impact the pelvic floor. Radiation, either external beam or internal brachytherapy, can cause fibrosis (hardening) in tissues of the pelvis, which may lead to narrowing and shortening in the vaginal canal. Fibrosis in the vaginal wall and pelvic floor musculature can manifest as incontinence and/or urgency of bowel and bladder, pelvic pain, and sexual dysfunction. 2,3,4 Studies have demonstrated that following surgery and radiotherapy for gynecologic cancers, patients are more likely to report lower libido, altered sexual response, change in body image, and distress related to changes in sexual health.5,6
Removal of pelvic lymph nodes also places patients at risk for developing lypmhedema, or chronic swelling. Dissection of the pelvic lymph nodes can lead to swelling in the abdomen, genitals, and legs. There is some evidence to suggest that genital lymphedema can impact bladder function 7, and it may have implications for sexual health as well.
The degree to which cancer treatment affects pelvic floor varies. Some patients may have no symptoms, and some may have multiple, severe impairments. Some issues may arise immediately following treatment, and some may take time to develop.
Why aren’t more people talking about pelvic floor health after cancer treatment?
There are many reasons why patients don’t get help for pelvic floor dysfunction right away. After cancer treatment, many patients are so grateful to have survived that they feel guilty complaining about these comparatively “minor” issues.6 Many patients are also not aware that pelvic floor treatment exists, or feel that they will just have to live with their symptoms. As a result, many patients suffer in silence –sometimes for years– before they receive the treatment they need. Patients are also very resilient, and find ways to deal with issues of bladder, bowel, and sexual dysfunction on their own. Everyone needs a little help sometimes, and specialized treatment exists to address cancer-related dysfunction of the pelvic floor.
What can I expect in pelvic floor rehabilitation?
At your first visit, your therapist will take a thorough history to better understand your complaints, establish goals for treatment, and to screen for conditions that require medical treatment. This will include your history with cancer, types of treatments you received, and symptoms you may have had prior to your treatment for cancer. Your therapist may then perform a physical examination to include movement, muscle strength, and range of motion. Pelvic floor physical therapy often requires a detailed examination of the pelvic floor. This can include internal or external examination, often both. Your therapist will talk you through the process of the pelvic examination and give you the opportunity to ask questions or express concerns. Your therapist will always make sure that you consent to the examination, and you can stop the exam at any point if you feel uncomfortable. The internal examination involves assessing the pelvic floor muscles manually, checking for strength, flexibility, and tone. The examination may reveal tender spots known as trigger points that refer pain to other areas of the body. The therapist will also assess for fibrosis or muscle spasm, and will check for normal range of motion in the pelvic floor muscles.
Based on the results of your examination, your therapist will provide treatment. Treatment might include pelvic floor strengthening, relaxation, muscle stretching, or trigger point treatment. Patients may need to use tools called dilators to stretch the vaginal tissues and soften fibrosis in the perineal region. Treatment might also include stretching for your legs and low back, breathing exercises, scar massage, bladder and bowel training, or establishing an exercise regimen. No two patients are alike, and the treatment protocols change based on the patient’s particular history, needs, and goals.
Pelvic floor rehabilitation is always based on a foundation of informed consent, and mutual trust between the provider and patient. Communication is of utmost importance, and your therapist should listen openly to your concerns, questions, goals, and observations. The success of pelvic floor rehabilitation is dependent on a correct assessment of the source of the dysfunction, the correct treatment plan provided by the therapist, and the patient’s adherence to the plan.
What’s next?
If you think you might have symptoms of pelvic floor dysfunction (or even if you just want to find out if you do), speak to your healthcare providers, gp, nurse or oncologist or can contact a pelvic health physiotherapist directly. There is care available for these issues that are sometimes difficult to discuss. With the right treatment, it is entirely possible to decrease or eliminate symptoms of pelvic floor dysfunction. Contact us with any questions you might have, to schedule your consultation!
About the Author: Lisa Cheek, PT, DPT, CLT-LANA
Lisa is a physiotherapst , certified Lymphedema therapist based in Colorado, USA. She is progressing through her pelvic health certification through the Women’s Health APTA. Her treatment philosophy emphasizes care for the whole person, and considering the big picture when treating musculoskeletal dysfunction. Lisa believes in empowering patients through education and incorporating principles of modern pain science.
References
Huffman LB, Hartenbach EM, Carter J, Rash JK, Kushner DM. Maintaining sexual health throughout gynecologic cancer survivorship: A comprehensive review and clinical guide. Gynecol Oncol. 2016;140(2):359-368. doi:10.1016/j.ygyno.2015.11.010Hazewinkel MH, Sprangers MAG, van der Velden J, et al. Long-term cervical cancer survivors suffer from pelvic floor symptoms: A cross-sectional matched cohort study. Gynecol Oncol. 2010;117(2):281-286. doi:10.1016/j.ygyno.2010.01.034Bergmark K, Åvall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal Changes and Sexuality in Women with a History of Cervical Cancer. N Engl J Med. 1999;340(18):1383-1389. doi:10.1056/NEJM199905063401802Bernard S, Ouellet M-P, Moffet H, Roy J-S, Dumoulin C. Effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area: a systematic review. J Cancer Surviv 2016;10(2):351-362. doi:10.1007/s11764-015-0481-8Rutledge TL, Heckman SR, Qualls C, Muller CY, Rogers RG. Pelvic floor disorders and sexual function in gynecologic cancer survivors: a cohort study. Am J Obstet Gynecol. 2010;203(5):514.e1-e514.e7. doi:10.1016/j.ajog.2010.08.004Hazewinkel M, Sprangers M, Taminiau-Bloem E, van der Velden J Burger M, Roovers J-P. Reasons for not seeking medical help for severe pelvic floor symptoms: a qualitative study in survivors of gynaecological cancer: Pelvic floor symptoms in survivors of gynaecological cancer. BJOG Int J Obstet Gynaecol. 2010;117(1):39-46. doi:10.1111/j.1471-0528.2009.02411.xBergmark K, Avall-lundqvist E, Dickman PW, Henningsohn L, Steineck G. Lymphedema and bladder-emptying difficulties after radical hysterectomy for early cervical cancer and among population controls. Int J Gynecol Cancer. 2006;16(3):1130-9.Image credits
1) http://www.drjenniferashton.com/





